Association of DTNBP1 With Schizophrenia: Findings From Two Independent Samples of Han Chinese Population
Yongfeng Yang 1,2,3?, Luwen Zhang 1,2,3?, Dong Guo 1,2,3, Lin Zhang 4, Hongyan Yu 1, Qing Liu 1,2,3, Xi Su 1,2,3, Minglong Shao 1,2,3, Men Song 1,2,3, Yan Zhang 1,2,3, Minli Ding 1, Yanli Lu 1, Bing Liu 5,6,7, Wenqiang Li 1,2,3, Weihua Yue 8,9, Xiaoduo Fan 10, Ge Yang 1,2,3* and Luxian Lv 1,2,3,11*
1 The Second Affiliated Hospital of Xinxiang Medical University, Henan Mental Hospital, Xinxiang, China, 2 Henan Key Lab of Biological Psychiatry, Xinxiang Medical University, Xinxiang, China, 3 Psychiatry Department, Affiliated Wuhan Mental Health Center, Tongji Medical College of Huazhong University of Science & Technology, Wuhan, China, 4 Affiliated Wuhan Mental Health Center, Tongji Medical College of Huazhong University of Science & Technology, Wuhan, China, 5 Brainnetome Center, Institute of Automation, Chinese Academy of Sciences, Beijing, China, 6 National Laboratory of Pattern Recognition, Institute of Automation, Chinese Academy of Sciences, Beijing, China, 7 University of Chinese Academy of Sciences, Beijing, China, 8 Institute of Mental Health, Peking University, Beijing, China, 9 Ministry of Health Key Laboratory of Mental Health, Peking University, Beijing, China, 10 Psychiatry Department, University of Massachusetts Medical School and UMass Memorial Medical Center, Worcester, MA, United States, 11 Psychiatry Department, Henan Provincial People's Hospital, Zhengzhou, China
Abstract
Objectives: Schizophrenia (SZ) is a complex psychiatric disorder that has a strong genetic basis. Dystrobrevin-binding protein 1 (DTNBP1) is one of the genes thought to be pivotal in regulating the glutamatergic system. Studies have suggested that variations inDTNBP1 confer susceptibility to SZ and clinical symptoms. Here, we performed a twostage independent verification study to identify polymorphisms of the DTNBP1 gene that might be associated with SZ in the Han Chinese population.
Methods: In stage 1, 14 single nucleotide polymorphisms (SNPs) were genotyped in 528 paranoid SZ patients and 528 healthy controls (HCs) using the Illumina GoldenGate assays on a BeadStation 500G Genotyping System. In stage 2, ten SNPs were genotyped in an independent sample of 1,031 SZ patients and 621 HCs using the Illumina 660k Genotyping System. Clinical symptoms were assessed using the Positive and Negative Syndrome Scale.
Results: There was a significant association related to allele frequency, and a trend association in relation to genotype between SZ patients and HCs at rs4712253 (p = 0.03 and 0.05, respectively). These associations were not evident following Bonferroni correction (p > 0.05 for both). Haplotype association analysis revealed that only two haplotypes (GAG and GAA; rs16876575-rs9464793-rs4712253) were significantly different between SZ patients and HCs (c2 = 4.24, 6.37, p = 0.04 and 0.01, respectively). In addition, in SZ patients there was a significant association in the rs4964793 genotype for positive symptoms, and in the rs1011313 genotype for excitement/hostility symptoms (p = 0.01 and 0.002, respectively). We found a significant association in the baseline symbol digital modalities test (SDMT), forward-digital span (DS), backward-DS, and semantic fluency between SZ patients and HCs (p < 0.05 for all). Finally, the SNP rs1011313 genotypes were associated with SDMT in SZ patients (p= 0.04).
Conclusion: This study provides further evidence that SNP rs4712253 of DTNBP1 has a nominal association with SZ in the Han Chinese population. Such a genotype variation may play a role in psychopathology and cognitive function.
Keywords: schizophrenia, DTNBP1, polymorphism, psychotic symptoms, cognition
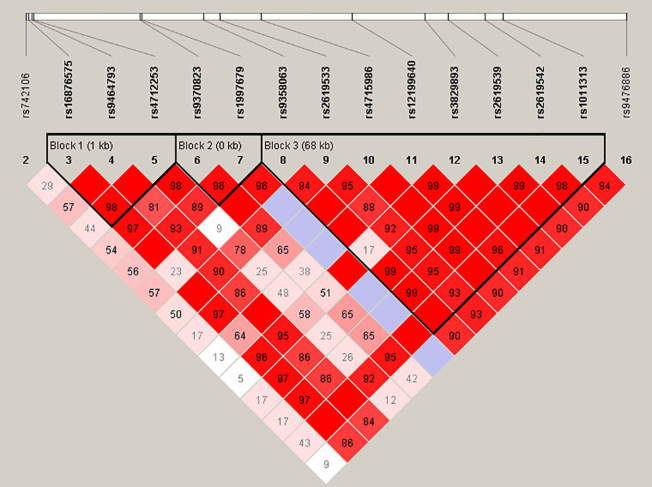 | FIG. Haplotype block structure of the DTNBP1 gene in both SZ patients and HCs in stage 1 and 2 samplese combined. The index association SNP is represented by a diamond. The colors of the remaining SNPs (circles) indicate LD with the index SNP based on pairwise r2 values from our data.
|
